For direct access to specialists
Refer to our provider manual and related materials online to confirm your state’s direct access referral requirements.
Some of your patients may have questions about their care and coverage as we approach the end of the 2025 plan year. This document may help you support patients with continuity of care, claims processing, and coverage transition questions.
GO TO:
A QHP is a plan that the Centers for Medicare & Medicaid Services (CMS) certifies and meets certain requirements under the Patient Protection and Affordable Care Act (ACA). QHPs have networks that are unique to ACA plans. QHP plans are also called exchange plans or Marketplace plans.
The date your patient’s plan starts depends on their sign-up date.
In most states, Open Enrollment runs from November 1 to January 15. Coverage usually starts on the first day of the month following the plan selection. For example, if your patient selects a plan on December 31, their coverage will start on January 1. California and New Jersey residents can enroll until January 31 for coverage starting February 1.
Your patients may qualify to get coverage outside of the Open Enrollment window if they’ve had a big life change or one coming up, such as a new child or the loss of their health plan.
To check a patient’s eligibility, use our Availity® online portal.
We’ve expanded to add more counties in these states we previously entered:
We also have plans in these states and counties:
Plan coverage area is subject to approval.
You can use our online provider search.
We encourage you to review our provider manuals and other helpful resources. They’re available online.
You can use the Provider Data Management (PDM) tool in the Availity® provider portal to update and maintain your profile. To learn more about the Availity portal, sign up for training and find resources like our PDM quick reference guide, visit our Availity resource center.
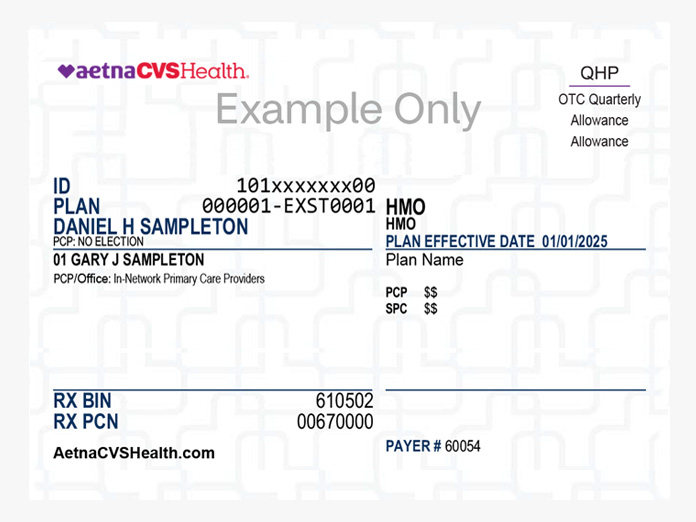
Exchange members have “QHP” on the upper right corner of their member ID card. The company logo is on the upper left corner of the card.
Here’s an example of a member ID card.
No matter where the member bought their plan, you will verify benefits, eligibility and the PCP on record as you normally do. With our Availity® provider portal, it’s easy to manage many tasks online. You can submit claims, check claim status and patient eligibility, request precertification, submit disputes and appeals, and more.
Use the number ending in “00” for the subscriber’s member ID number. Submitting requests (such as a claim or prior authorization request) for someone other than the subscriber? Replace the “00” with the last two numbers for that person.
Here’s an example:
Subscriber (Joseph Smith) - 10XXXXXXXX00
Dependent 1 (Jane Smith) - 10XXXXXXXX01
Dependent 2 (Daniel Smith) - 10XXXXXXXX02
Yes. That’s because members don't have out-of-network benefits with any plan, in any state, except for emergencies.
These specialties allow direct access* and may not require referrals. Some services may require precertification.*
To find providers in the exchange network, use our provider search.
ACA individual insurance plans only coordinate with Medicare coverage. If a member is eligible for and elects Medicare, then Medicare will always be primary.
Individual insurance plans use Government Exclusion (GE) to coordinate with Medicare. GE is a way to determine Aetna payment when Medicare is the member’s primary insurance. We exclude Medicare payments from the total allowed charges. Aetna CVS Health considers the allowance based on the member’s responsibility after Medicare has considered the claim.
We automatically assign most members a PCP except for those in Missouri, New Jersey, North Carolina and Virginia (Aetna CVS Health members in Roanoke and Richmond). Members can also call us to choose their PCP. Then we’ll mail them a new ID card.
Aetna CVS Health plans don’t include out-of-network benefits in any state, except for emergencies. When we approve coverage, it’s at the in-network benefit and at a contracted rate (for broad network providers) or negotiated in a letter of agreement.
MinuteClinic® locations and some labs have a national network. We don't consider them out of network even if they're outside of the service area.
To find state formulary information and other drug coverage resources, choose a state:
Yes, the payer ID and claim address are the same for exchange plans. For information on electronic claims submission, review our claims, payment and reimbursement resources.
We encourage electronic claims submission. Prefer to mail a claim? Use one of these addresses:
No. The current claims filing limits are the same. For guidance on filing standards, go to insurance regulations by state.
That means we’ll continue to pay claims from the first month of non-payment. This grace period is different for members who receive premium subsidies and those who don’t:
Need to find out if a member is in a grace period?
To check benefits and eligibility, log in to Availity. You’ll find “HIX Grace Period” under Plan/Product if the member is in a grace period.
We process out-of-network claims based on the member’s plan benefits. If the member has assigned benefits, we pay you directly. Members don’t have out-of-network benefits with any plan, in any state, except for emergencies.
We’ll reimburse you as outlined in:
For details, check your contract agreement or amendment.
For direct access to specialists
Refer to our provider manual and related materials online to confirm your state’s direct access referral requirements.
For services that require precertification
Some services and equipment require prior approval, including durable medical equipment, hospital ambulatory surgery, hospital outpatient and radiology and pathology and lab. To confirm benefits, you can call your provider support team at 1-888-632-3862 (TTY: 711).
Health plans are offered or underwritten or administered by Aetna Health of California Inc., Aetna Health Inc. (Florida), Aetna Health Inc. (Georgia), Aetna Life Insurance Company, Aetna Health of Utah Inc., Aetna Health Inc. (Pennsylvania), or Aetna Health Inc. (Texas) (Aetna). Aetna, CVS Pharmacy and MinuteClinic, LLC (which either operates or provides certain management support services to MinuteClinic-branded walk-in clinics) are part of the CVS Health® family of companies.
Providers are independent contractors and are not agents of Aetna. Provider participation may change without notice. Aetna does not provide care or guarantee access to health services. Information is accurate as of the production date; however, it is subject to change.
Health benefits and health insurance plans contain exclusions and limitations.
Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites.
You can visit the Health Insurance Marketplace® to shop for ACA individual & family plans, sign up, and see if you qualify for premium and plan savings.
You can visit the Nevada Health Link to shop for ACA individual & family plans, sign up, and see if you qualify for premium and plan savings.
You can visit Covered California to shop for ACA individual & family plans, sign up, and see if you qualify for premium and plan savings.
You can visit Get Covered New Jersey to shop for ACA individual & family plans, sign up, and see if you qualify for premium and plan savings.
You can visit the Health Insurance Marketplace® to shop for ACA individual & family plans, sign up, and see if you qualify for premium and plan savings.
The guest payment feature of our bill payment system is currently not available. You can still make an online payment by logging in to your member website. Payments can also be made by calling the number on the back of your ID card. We are working on a resolution and appreciate your patience.
You can visit Maryland Health Connection to shop for ACA individuals & family plans, sign up, and see if you qualify for premium and plan savings.
You can visit Virginia's Insurance Marketplace to shop for ACA individuals & family plans, sign up, and see if you qualify for premium and plan savings.
Remember to stop back on November 1 during Open Enrollment to choose your 2024 plan.
Had a big life change? You may still be able to get coverage for 2023 if you qualify.