For walk-in clinic locations
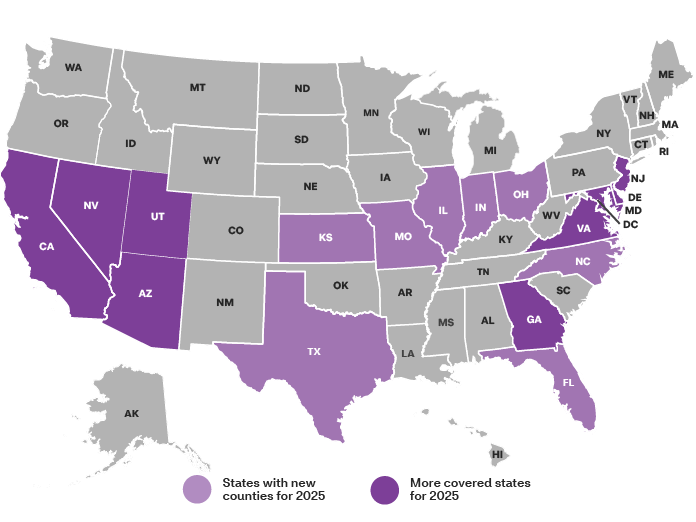
For a list of participating walk-in clinics, use our online provider search tool. Includes select MinuteClinic services. Not all MinuteClinic services are covered or may be covered at negotiated contract rates. Not available in all states. Walk-in appointments are not guaranteed. Online scheduling recommended. Check your plan documents for more details. Members enrolled in qualified high-deductible health plans must meet their deductible before receiving covered primary care or non-preventive services at no cost share.